Research in Progress
The Carlton Research Group is committed to increasing diversity in science and is invested in the full participation of historically under-represented groups in public health research and practice. We are a multi-disciplinary group including masters and doctoral students, and postdoctoral fellows. We strive to provide an engaging, collaborative work environment.
Current projects

Reemergence and persistence of schistosomiasis in China
China has achieved remarkable progress in the control of schistosomiasis, a water-borne pathogen that causes liver fibrosis, anemia and can impair child growth and development. However, schistosomiasis has reemerged and persists in some areas, despite aggressive disease control efforts. We are working with collaborators at the Sichuan Center for Disease Control and Prevention in order to understand why these pockets of transmission persist. In our research over the last several years, we have demonstrated that infections tend to be concentrated in a limited number of individuals, and have developed an efficient method for sequencing large numbers of loci from field-collected S. japonicum miracidia. We have also found that the agricultural practice of using human and animal waste as an agricultural fertilizer (often called night soil), may facilitate transmission in human populations, as well as transmission in bovine populations. Our team has also recently employed remote sensing and geospatial analytical tools to evaluate best-practice schistosomiasis surveillance efforts within low-transmission environments. We evaluated the role of travel in schistosomiasis exposure and infection risk (in our study villages where some people regularly travel to cities, we found more travel was associated with reduced water contact and infection risk). Current efforts are underway to understand the roles of parasite import and export along social and hydrological gradients as sources of infection in residual transmission hotspots.
.jpg?sfvrsn=f43bc6b9_0)
COVID-19 surveillance and modeling
At the onset of the COVID-19 pandemic in March 2020, our group became a core part of the COVID-19 Modeling Group. This team used modeling, data analysis, and rapid evidence synthesis to inform state and local officials in Colorado about the current state and possible future trajectories of the pandemic. In 2022, with funding from the Council of State and Territorial Epidemiologists (CSTE), our team expanded its focus to developing modeling tools and data visualizations to meet the needs of public health leaders in the Rocky Mountain West (RMW), comprising Colorado, Idaho, Montana, New Mexico, Utah, and Wyoming. We launched and maintained a website from the end of the COVID-19 public health emergency through December 2023 providing interactive COVID-19 data visualizations and summaries of emerging topics for COVID-19 planning and response in the RMW. This website was developed following interviews with public health officials across the RMW region to assess their needs during a transitional period in the pandemic response. Our current work includes efforts to improve surveillance and modeling tools for pandemic pathogens, estimate the impact of climate on respiratory pathogens, and to improve our understanding of how epidemics spread between urban, rural, and resort communities.

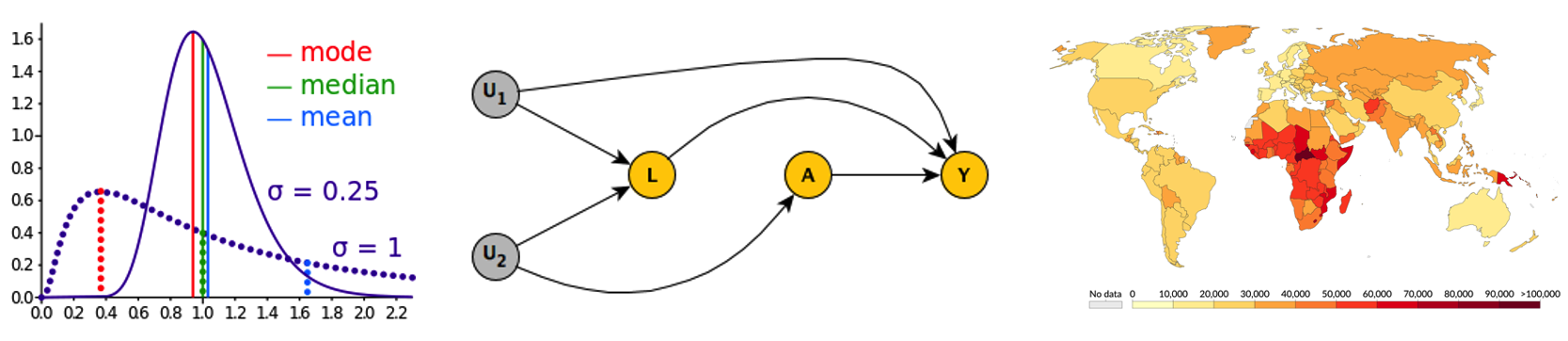
Impacts of climate change on water-borne disease
There is strong evidence that climate impacts the distribution of water-borne diseases. The causal pathways are complex, and health impacts of climate change depend not only on meteorological exposures but other underlying vulnerabilities. We are interested in improving our understanding of these casual pathways so that we can identify locations and time windows of elevated risk and ultimately, design design interventions and early warning systems to reduce the burden of water-born diseases in a changing climate. Our early work in this area includes a systematic review, a meta-analysis, and a proposed framework to characterize the relationships between climate drivers, including temperature, heavy rainfall, flooding, and drought, and their relationship with infectious diarrhea. More recently, our work has included a study estimating the impact of weather on the use of safe and unsafe drinking water in countries in Asia and Africa; and a study of the impact of precipitation and temperature on giardia and cryptosporidiosis in Colorado.
Training for communicable disease epidemiologists
The Carlton Research Group provides training and educational seminars for communicable disease epidemiologists at state and local health departments around Colorado. Topics are anchored in the context of infectious diseases and have included epidemiology, biostatistics, the health impacts of climate change, and the use of mathematical modeling to inform pandemic policy. We strive to create engaging educational experiences through trainings that include foundational concepts, real-world examples, and connection to additional resources for further learning. We seek to deepen our relationships with existing connections as well as forge new connections with other potential organizations seeking to train their staff in infectious disease epidemiology. For more information on past and future trainings given by our research group, please contact Emma Wu at [email protected].


