Lessons Learned Already: COVID-19
Mar 13, 2020
Yes, of course I am writing about the pandemic of coronavirus disease 19 (COVID-19) caused by the severe acute respiratory syndrome-coronavirus 2 (SARS-CoV-2). This disease has emerged in the United States since my last comments, only a month ago. In February’s commentary, the epidemic was a footnote; now, it is a flashing headline. Over the month, COVID-19 has popped up throughout most of the United States, quickly altering our lives in so many ways. The consequences are sweeping and I do not need to list them all--as we are living through this crisis together. For the Colorado School of Public Health and our partner universities, steps have been taken to protect the health of students, staff, and faculty, including the curtailment of travel and the switch from in-class instruction to online.
When public health works, it is in the background and overlooked. When challenged by epidemics or other disasters, it is in the foreground with expectations of controlling and ending problems. Explaining what public health is can be difficult, as the two words—public health—capture an extraordinary scope of activities. But at the moment, explanation is neither difficult nor needed. Similarly, the word “epidemiology” has become common parlance. The best description of being on one of the COVID-19 cruise ships was: “an epidemiological nightmare.”
Most of the methods used to combat the epidemic have long been used: contact tracing, quarantine, and social distancing, now augmented by molecular characterization of the virus and computer modeling. Note, however, that the principles underlying elegant population models of the COVID-19 epidemic are almost a century old, dating to the Reed-Frost theory of epidemics, developed in 1928 by these two faculty members at the then Johns Hopkins School of Hygiene and Public Health, and described by Helen Abbey in a 1952 paper. And, the COVID-19 epidemic is following the historical track of its many successors: the search for explanation, blame, and a tortuous path towards control.
Sadly, there is much to learn from the handling of this pandemic. Our “post-truth” world slowed the needed national response as the epidemic was dismissed as a “hoax”, politicized, and trivialized, while the threat was undeniably growing. Even within the last week, some administration officials communicated irresponsibly and sometimes contradicted the messaging by the nation’s experts. In his March 11 speech to the nation, President Trump described SARS-CoV-2 as a “foreign virus”, an effort appearing to explain by blame. In today’s world, all infectious agents need to be regarded as potentially global; they don’t acknowledge national borders. Perhaps abetted by the Administration, misinformation has spread as rapidly as COVID-19; the phrase “viral spread” via the internet could not be more apt. The false information adds to the challenge of helping the public to understand what to do and to take the right steps.
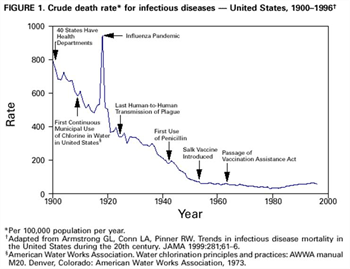
Epidemics do end, but this one will have lasting impact—memories and fears, losses of jobs and savings, and more. Some will wonder, for example, what team might have come out on top of “March Madness”? Others will remember losses of family and friends. Let’s hope that the case-fatality rate is not high and that our protective measures and medical care are effective. For a reminder of what happened in the 1918 influenza epidemic, see the figure below. For more on that epidemic and lessons learned, still resonating today, read John Barry’s The Great Influenza.
While we await the end of this epidemic, the Colorado School of Public Health is actively engaged. In February, faculty from the Department of Epidemiology hosted a panel discussion for members of the CU Anschutz community that addressed the virus. Glen Mays, Professor and Chair of the Department of Health Systems, Management and Policy, directs the National Health Security Preparedness Index, which provides information about states’ health emergency preparedness levels. He has been at the forefront of media coverage on coronavirus preparedness at the local and national level. Members of our epidemiology faculty have also been speaking with the media, providing the public with information about virus risks, spread, and precautions.
As a reminder, resources and publications on the COVID-19 pandemic can be found at the following:
- CDC
- The New York Times
- The Lancet
- New England Journal of Medicine
- Johns Hopkins University
- Journal of the American Medical Association
- Worldometer

Jonathan Samet, MD, MS
Dean, Colorado School of Public Health